Select your destination
Continue to Radiometer Medical
Procalcitonin (PCT) – the biomarker of choice to aid in the diagnosis of sepsis
Procalcitonin is regarded as a biomarker with both diagnostic and prognostic impact, offering emergency department and intensive care clinicians a key tool to aid in the diagnosis of sepsis, and thereby improve antibiotic decision-making and potentially improve clinical outcomes [1].
Procalcitonin (PCT), a 116–amino acid polypeptide prohormone of calcitonin, has emerged as a biomarker to aid in the diagnosis of sepsis and with a high potential to improve the clinical assessment of patients [1].
PCT is synthesized primarily by the C-cells of the thyroid gland, and to a lesser extent in the neuroendocrine tissue of other organs such as the lungs and intestines. Normal procalcitonin levels in the blood are very low.
However, production can be stimulated in almost every organ by inflammatory cytokines and especially bacterial endotoxins present e.g. during sepsis, causing high amounts of procalcitonin to be released in the blood.
This allows procalcitonin levels to be used as a biomarker of e.g. sepsis. The higher the level of PCT, the greater the likelihood of systemic infection and sepsis [2].
The favorable kinetics of PCT potentially enable earlier diagnosis of sepsis and better monitoring of its progression. The primary utility of PCT is therefore to help uncover the presence of systemic bacterial infections such as sepsis, and numerous studies have investigated the potential roles of PCT in diagnosis and management of e.g. sepsis [2-4].
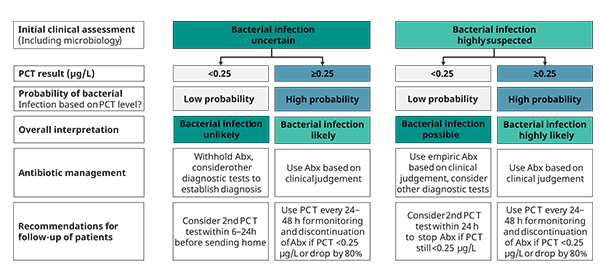
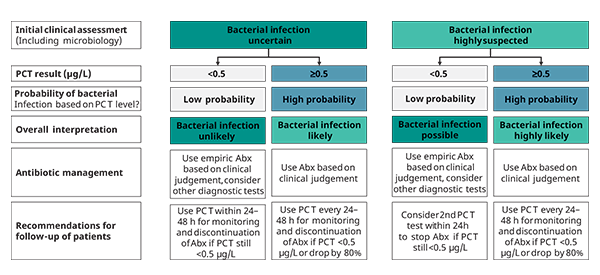
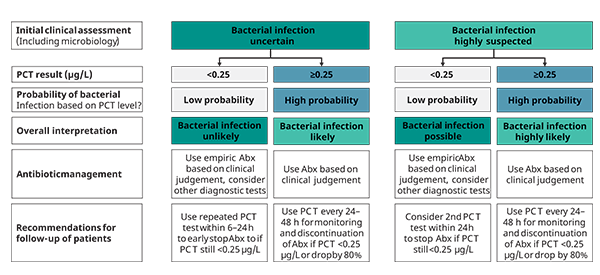
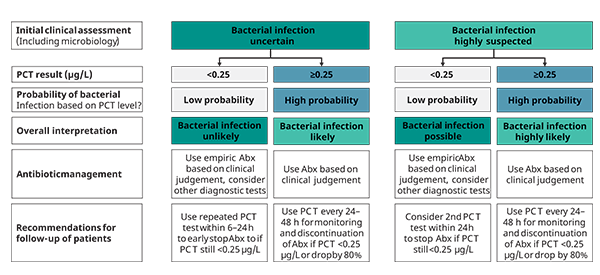
A recent consensus paper by Schuetz et al. offers recommendations on antibiotic management of patients in ED and ICU based on clinical severity, probability of bacterial infection and PCT levels. See figures 1 - 3 [1].
Growing evidence for using PCT as a diagnostic biomarker for early detection of sepsis
Currently there is no recognized diagnostic test available for sepsis diagnosis as stated by the Sepsis-3 task force [5].
The recognition of sepsis requires careful patient monitoring and observation. This philosophy is also found in the Sepsis Six initiative [6], NICE Guideline NG51 [7], and 2018 sepsis bundle [8], which is a combination of both monitoring and proactive measures that should be performed within an hour, one of them being administering empiric intravenous antibiotics.
During the past decade, the role of biomarkers to assist in the diagnosis and management of infections and sepsis has been extensively explored. The measurement of procalcitonin is now commonly used in many parts of the world to assist in the diagnosis of e.g. sepsis and to help define the duration of antimicrobial therapy [9].
Compared to C-reactive protein (CRP)—another biomarker frequently used to aid in the diagnosis of systemic inflammation and infection—procalcitonin has superior biokinetics, characterized by concentrations increasing earlier in the event of bacterial infection and sepsis, and decreasing faster in case the infection is controlled [10].
PCT-guided use of antibiotic therapy
The use of PCT is described in the Surviving Sepsis Campaign guidelines [9], with the suggestion that PCT could be used for antimicrobial stewardship. It would be advisable to measure PCT in the diagnostic phase of sepsis, to have an initial baseline PCT value, before antibiotics are administered [11].
Empiric antibiotic therapy should be initiated immediately, and the patient referred to ICU in the suspicion of sepsis. It is recommended to repeat the PCT testing regularly to ensure that the patient is responding to the treatment (fig. 1-3).
De-escalation of antimicrobial therapy is a mainstay of antibiotic stewardship programs and is associated with less resistant microorganisms, fewer side effects, and lower costs (SSC guidelines 2016) [9].
SSC guidelines 2016 suggest that measurement of procalcitonin levels:
- can be used to support shortening the duration of antimicrobial therapy in sepsis patients
- can be used to support the discontinuation of empiric antibiotics in patients who initially appeared to have sepsis, but subsequently have limited clinical evidence of infection
A number of clinical studies have proven the effectiveness and safety of PCT-guided therapy [3, 12, 13-16]. Guided by PCT measurements, the duration of ABx in patients in both ED and ICU settings was shortened consistently by several days, without compromising clinical safety [11, 13, 15, 16].
References
1.Schuetz P. et al. Procalcitonin (PCT)-guided antibiotic stewardship: an international experts consensus on optimized clinical use. Clin Chem Lab Med 2019; 57, 9.
2. Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: Clinical utility and limitations. Crit Care Med 2008; 36,
3. Tang H, Huang T, Jing J, Shen H, Cui W. Effect of procalcitoninguided treatment in patients with infections: a systematic review and meta-analysis. Infection 2009; 37.
4. Jones AE, Fiechtl JF, Brown MD, Ballew JJ, Kline JA. Procalcitonin test in the diagnosis of bacteremia: a meta-analysis. Ann Emerg Med 2007; 50.
5. Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315, 8.
6. Daniels, R.; Nutbeam, T.; McNamara, G.; Galvin, C. The sepsis six and the severe sepsis resuscitation bundle: A prospective observational cohort study. Emerg. Med. J. 2011, 28.
7. National Institute for Health and Care Excellence. Sepsis: Recognition, Diagnosis and Early Management (NICE Guideline NG51). 2016. Available online: https://www.nice.org.uk/guidance/ng51 (last accessed June 2020)
8. Levy, MM. Evans, LE. Rhodes, A. The surviving sepsis campaign bundle: 2018 update. Crit. Care Med. 2018; 46.
9. Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med 2017; 43, 3.
10. Meisner M, Tschaikowsky K, Palmaers T, Schmidt J. Comparison of procalcitonin (PCT) and C-reactive protein (CRP) plasma concentrations at different SOFA scores during the course of sepsis and MODS. Crit Care 1999; 3.
11. Broyles M. Impact of Procalcitonin-Guided Antibiotic Management on Antibiotic Exposure and Outcomes: Real-world Evidence. Open Forum Infectious Diseases 2017.
12. Balk RA et al. Effect of procalcitonin testing on health-care utilization and costs in critically ill patients in the United States. CHEST 2017; 151.
13. Christ-Crain M, Stolz D, Bingisser R et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 2006; 174.
14. Schuetz P, Briel M, Christ-Crain M et al. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis 2012; 55.
15. Christ-Crain M, Jaccard-Stolz D, Bingisser R et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, singleblinded intervention trial. Lancet 2004; 363.
16. Bouadma L, Luyt C-E, Tubach F et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 2010; 375.
Cookies are used on this website
Use of cookiesPlease enter a valid email
We will be sending an e-mail invitation to you shortly to sign in using Microsoft Azure AD.
It seems that your e-mail is not registered with us
Please click "Get started" in the e-mail to complete the registration process
Radiometer is using Microsoft AZURE Active Directory to authenticate users
Radiometer uses Azure AD to provide our customers and partners secure access to documents, resources, and other services on our customer portal.
If your organization is already using Azure AD you can use the same credentials to access Radiometer's customer portal.
Key benefits
- Allow the use of existing Active Directory credentials
- Single-sign on experience
- Use same credentials to access future services
Request access
You will receive an invitation to access our services via e-mail when your request has been approved.
When you accept the invitation, and your organization is already using AZURE AD, you can use the same credentials to access Radiometer's customer portal. Otherwise, a one-time password will be sent via e-mail to sign in.